Beyond the microscopic lens …
The ongoing COVID-19 pandemic has once again turned the spotlight on to pathologists and laboratory medicine, not to miss out the indispensable role of microbiologists, virologists and biochemists. Now more than ever, their role can be compared to that of a film director, who remains behind the scene but calls the shots!
By now we all know that blood samples and naso and oropharyngeal swabs are been collected by PPE clad, trained laboratory professionals for COVID-19 testing. But have you ever wondered what happens after you give your samples? How are the various results arrived at? How does the Doctor arrive at a treatment plan based on these numbers? It is the pathologist and his team of trained clinical laboratory personnel who don the hats of both a physician and a scientist to give all answers.
Pathology - the backbone of medicine
Pathology is a marvelous medical science that underpins every aspect of patient care, from diagnosis, monitoring and interpretation of clinical findings. There’s not really any clinical department of the hospital that doesn’t rely on pathology in some capacity. A pathologist has the ultimate responsibility for the test results, the quality and safety standards of the laboratory, advising clinicians on the interpretation of test results and further investigation of the patient. Needless to say, the primary data for most disease diagnostics comes from pathology, and pathologists are often among the most informed about an individual patient’s disease.
The last century has witnessed a significant reduction in cases of illnesses such as polio across the world, as well as considerable advances in blood transfusion, vaccination and treatment of inherited conditions. These developments are all thanks to the pioneering work of pathologists.
The broad range of services provided by pathologists to virtually every part of clinical medicine is an appealing feature for physicians-in-training. Those with a penchant for problem-solving are drawn towards the intellectually endowed field.
With the growth of healthcare industry and emphasis being laid on annual health check ups, the demand for laboratory testing has grown enormously. For this, hospitals tie-up with chain of pathology laboratories which are mushrooming in every corner of cities. Due to the competition, it became essential to upgrade the quality and safety standards of the laboratory. As a result, an increasing number of hospitals and laboratories are now following the MCI / NABH / NABL / CAP accreditation guidelines for accurate and reliable diagnosis.
The frontline heroes
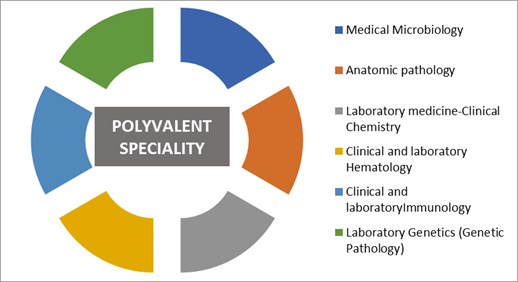
A pathologist is responsible for directing the lab functioning, interpreting results and giving diagnostic opinion to the clinician to help them decide treatment regimen. The role of a pathologist encompasses multiple fields. A pathologist is expected to demonstrate polyvalent skills including Microbiology, Biochemistry, Hematology, Immunology, Molecular Biology/Genetics.
Due to the crunch in the number of qualified MD pathologists, the Medical Council of India has decided to enable non-medical personnels with M.Sc. in Medical Biochemistry/Medical Microbiology or with a Ph.D. degree in Biochemistry, Microbiology, Biotechnology or Genetics to sign the technical report stating test results without recording any medical opinion.
Microbiologists in demand, thanks to COVID-19
The recent pandemic has brought forth the role of microbiologists and virologists. The rampant application of RT-PCR tests for confirmatory diagnosis has shifted focus on the microbiologists and virologists.
To some extent it has exposed the vulnerabilities of the healthcare sector, on giving less emphasis to microbiology as a sub-branch. India has been shifting its priorities with regards to medical microbiology research. While the focus has been on HIV, TB and now COVID-19, funding has been limited. Intensified research in microbiology could have led to development of indigenous diagnostic tests, however, limited funding and dependency on imports has been the main roadblocks.
Does that mean that a a microbiologist or biochemist can easily replace a pathologist?
Well, the answer is no. A microbiologist is an expert in differentiating the micro-organisms and their anti-microbial testing. On the other hand, a biochemist is the best person to take a call on lipid/liver profile tests and metabolic disorders and compare the results with established lab specific reference ranges.
A pathologist on the other hand, is responsible for selection of the appropriate laboratory test based on its usage purpose eg. screening or confirmatory and its clinical performance, based on prevalence, sensitivity, specificity, efficiency, and predictive value. For eg., if the risk associated with failure to diagnose a particular disease is high, false-negatives are unacceptable and only a test with high sensitivity is acceptable. Similarly, if a disease is potentially fatal and there is no therapy available, other than supportive care, false positive tests would be unacceptable and a test with high specificity would be desirable. In general, laboratory tests with both high sensitivity and specificity are desirable since both false-negatives and false-positives are equally unacceptable under most clinical circumstances. This is where the role of a pathologist becomes crucial in deciding on the test to be used.
An indispensable profession
In the current age of outcome-oriented medicine, pathologists can no longer employ the ‘shotgun approach’ and are expected to adopt ‘rifle’ (or targeted) approach for conducting laboratory tests. They need to lay emphasis on understanding the principles for selecting the most rational test on a patient. This judicious use of laboratory tests is critical to good laboratory practice and patient outcomes.
Techniques that a few years ago were available only for research are now ready for everyday clinical use. The trend is evident in the growing implementation of mass spectrometry and molecular diagnostics for clinical testing to provide same-day measurements of nucleic acids, proteins, and therapeutic drugs.
The growth of new technologies that produce biomedical “big data” (next-generation sequencing, multiparameter/multiplex flow cytometry, high throughput proteomics and metabolomics, systems biology analysis) has caused pathologists to reassess the best approach to diagnostics.
Budding pathologists need to be the drivers of technological development, rather than just reacting to the presence of new technologies in diagnostics. Technological advancements should be considered as an adjunct to the vital role played by pathologists not as a substitute. Electronic Medical Records (EMR), can help a pathologist consult a large number of patients remotely across a large geographic area. Point of Care devices are gaining popularity too. Though effective as a first line diagnostic tool, they should not be regarded as a substitute to a much more detailed analysis given by a pathologist. High throughput automation when combined with electronic identification technologies, provides a platform for the reduction of laboratory test- related medical errors and thus be of great help to pathologists to achieve a higher level of accuracy than that attained by manual processes.
Therefore, while we recognize that lab automation holds the key to enhanced diagnostics, it is necessary to acknowledge the indispensable role played by lab experts, be it the non medico team or pathologists.







Comments
Post a Comment